Leaders in Quality Care

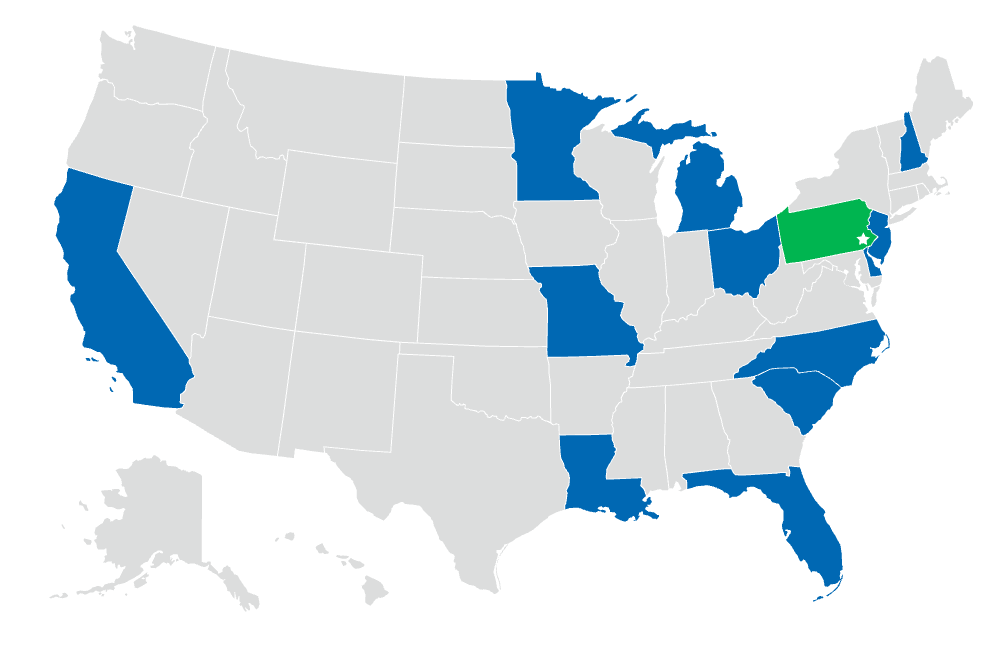
AmeriHealth Caritas has helped low-income and chronically ill populations since our inception in 1983.
Today, we are:
- One of the largest Medicaid managed care organizations in the United States. We touch the lives of millions of people through a philosophy of care that is comprehensive, compassionate, and outcomes driven.
- Improving the stability and predictability of Medicaid spending while sustaining quality health outcomes. We have a proven track record of prioritizing preventive care and reducing potentially preventable emergency room visits and hospital admissions. We also offer unique incentive programs that reward our providers for timely, efficient, equitable care, positive patient outcomes, and total cost of care reductions.
- Helping patients better manage their conditions and stay healthy through an integrated, person-centered approach to care coordination and management. Our disease-specific interventions have been effective at improving health outcomes for engaged members, while decreasing costs related to potentially preventable events.
Leaders in quality outcomes
We have more than 40 years of experience working with states to develop health care solutions tailored to our members’ individual needs. These solutions have a successful track record of improving health outcomes and reducing preventable hospital admissions:1
- 23% increase in professional visits over a three-year period for ongoing or preventive care (2020 – 2022):
- Specialty visits for members with chronic conditions increased by 44%.
- Primary care visits increased by 8% over two years (2021 – 2022).
- 20% decrease in emergency room visits (2020 – 2022):
- Potentially preventable emergency room visits decreased by 35%.
- 50% decrease in potentially preventable inpatient admissions over two years (2021 – 2022).
Cost-saving care
Medicaid managed care saves money
Evidence-based, coordinated managed care models like ours help maximize cost savings while delivering quality health care. As such, they have become a priority for state and federal policymakers.
With our expertise in integrated managed health care plans, preventive care, and community-based services, we are well positioned to help your government health agencies find the value you need.
Supporting high-risk members: decreasing inpatient admissions by 43%
AmeriHealth Caritas created a program for Medicaid members who are high utilizers of inpatient services, most of whom have both physical and behavioral health needs and face significant barriers to care. Our staff connected with members in person (e.g., on home visits) to support them in overcoming those barriers and to connect them with their behavioral health managed care organization. Members involved in the program experienced:2
- Improved adherence to treatment plans
- Better clinical outcomes
- A decrease in unnecessary care expenditures
- A 43% or greater decrease in inpatient admissions
Following our successful pilot, we integrated this program into all of our health plans.
Innovative solutions
To help drive equity, we’re always looking for new ways to bring superior care and support to our communities, members, and providers, and provide effective solutions for our government partners:
- National Committee for Quality Assurance (NCQA) Health Equity Accreditation
- Health Equity Committee and parity work
- Cultural responsiveness programming across the enterprise
- Provider health equity education
- Listen. Learn. Lead. — scaling best practices from high-equity providers in Black maternal care
- Doula coverage and maternal care coordination services
- Community-based organization (CBO) network — working with CBOs to address health inequities at the community level
- For Medicaid members receiving complex care management, 2020 – 2022.
- For all members, 2021 – 2024, AmeriHealth Caritas health outcomes evaluation platform, July 9, 2024.